Decoding Cushing Syndrome: Symptoms, Causes, and Treatments
Cushing syndrome is a complex condition that often leaves patients with more questions than answers. Whether you’re dealing with this syndrome yourself, or researching to support someone you care about, understanding the nuances of this condition is crucial. In this comprehensive guide, we’ll break down everything you need to know about Cushing syndrome—from its causes to diagnosis and treatment options—empowering you with the knowledge to navigate this journey.
What is Cushing Syndrome?
Cushing’s condition arises when there is an abnormally high level of glucocorticoids, such as cortisol, in the body for an extended period. These hormones are essential for managing stress and regulating metabolism, but when in excess, they can severely affect the body’s systems.
Cortisol, the primary hormone involved in this condition, is produced by the adrenal glands located above the kidneys. This hormone plays a key role in several functions, including:
- Increasing metabolism
- Raising blood glucose levels
- Supporting cardiovascular health
- Reducing inflammation
However, when cortisol levels remain elevated over time, it can lead to the onset of Cushing syndrome, presenting with a wide range of symptoms and complications.
Understanding the Hypothalamic-Pituitary-Adrenal (HPA) Axis
To grasp the underlying mechanisms of Cushing syndrome, it’s important to understand the HPA axis. This intricate feedback loop involves three key players:
- Hypothalamus: Releases corticotropin-releasing hormone (CRH).
- Pituitary Gland: Responds to CRH by producing adrenocorticotropic hormone (ACTH).
- Adrenal Glands: Stimulated by ACTH to release cortisol.
This feedback system ensures that cortisol levels remain balanced. When cortisol levels rise, they inhibit the release of CRH and ACTH through negative feedback. In Cushing syndrome, this balance is disrupted, leading to excessive cortisol levels.
What Causes Cushing Syndrome?
The causes can be remembered using the mnemonic “CAPE”:
- C: Cushing’s Disease (pituitary adenoma secreting ACTH)
- A: Adrenal adenoma (tumor producing excessive cortisol)
- P: Paraneoplastic syndrome (e.g., ACTH-secreting small cell lung cancer)
- E: Exogenous steroids (long-term use of corticosteroids like prednisone)
It’s important to distinguish between Cushing’s Disease and Cushing’s condition. The former specifically refers to a pituitary adenoma that leads to an overproduction of ACTH, while the latter encompasses a wider range of causes.
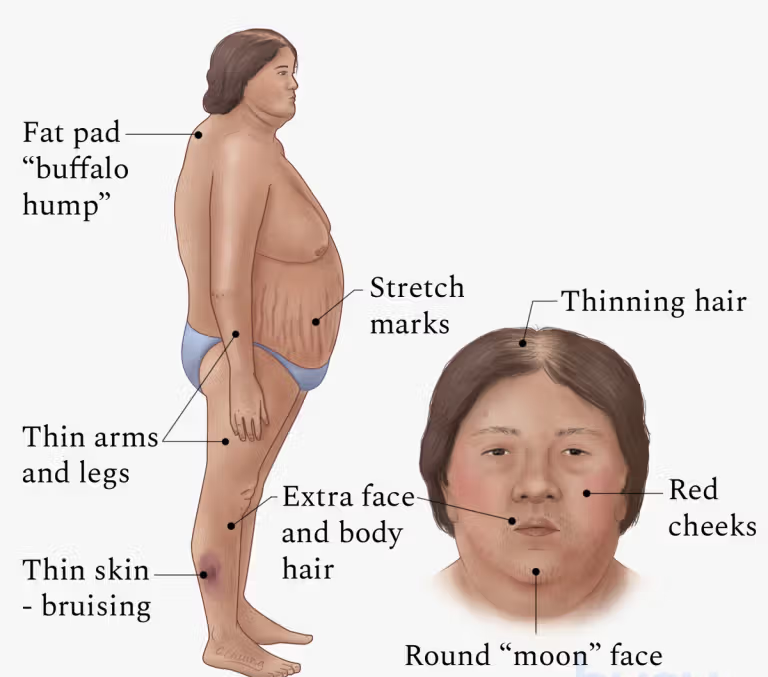
Symptoms of Cushing Syndrome
The symptoms can significantly impact quality of life. Here’s what to watch for:
- Physical Changes:
- Round, moon-shaped face
- Central obesity
- Abdominal stretch marks (striae)
- Buffalo hump (fat pad on upper back)
- Thin limbs with muscle weakness
- Skin and Hair Issues:
- Easy bruising
- Slow wound healing
- Excess facial hair in women (hirsutism)
- Mental Health:
- Anxiety
- Depression
- Insomnia
- Metabolic Effects:
- Hypertension
- Type 2 diabetes
- Osteoporosis
If these symptoms sound familiar, consulting a healthcare provider for further evaluation is critical.
Diagnosing Cushing Syndrome
Accurate diagnosis is a cornerstone of effective treatment. Here are the most common diagnostic methods:
1. Dexamethasone Suppression Test
This test involves administering a synthetic glucocorticoid (dexamethasone) to observe how cortisol levels respond. In normal individuals, dexamethasone suppresses cortisol production via negative feedback. In Cushing syndrome, cortisol levels remain high despite suppression attempts.
2. 24-Hour Urinary Free Cortisol Test
This test measures the total cortisol excreted in the urine over a 24-hour period. Elevated levels suggest Cushing syndrome but do not reveal the underlying cause.
3. Imaging Tests
- MRI of the brain: Detects pituitary adenomas.
- CT scans: Identify adrenal tumors or ectopic ACTH-producing tumors (e.g., lung cancer).
Treatment Options for Cushing Syndrome
1. Treating the Cause
- Surgery: The gold standard for removing pituitary adenomas, adrenal tumors, or ACTH-producing tumors.
- Adrenalectomy: Surgical removal of the adrenal glands if other interventions fail.
2. Medication
- Ketoconazole and metyrapone: Reduce cortisol production.
- Mitotane: Destroys adrenal cortex cells, lowering cortisol levels.
3. Lifelong Hormone Replacement
In cases where both adrenal glands are removed, patients require lifelong glucocorticoid and mineralocorticoid replacement therapy.
Managing Life with Cushing Syndrome
Living with Cushing syndrome can be challenging, but proactive management makes a difference. Key steps include:
- Regular Monitoring: Follow up with your healthcare provider for ongoing evaluation.
- Healthy Lifestyle: Prioritize a balanced diet, regular exercise, and stress reduction techniques.
- Support Networks: Engage with patient advocacy groups to connect with others navigating similar experiences.
Prognosis and Recovery
The outlook for Cushing syndrome depends on its cause and how promptly treatment begins. Surgical interventions often yield positive outcomes, but ongoing management is vital to prevent complications.
Understanding the Path Ahead
Cushing syndrome significantly impacts the body and mind, demanding attention and care. By understanding its symptoms, causes, and treatment options, you’re better equipped to take control of your health or support a loved one through their journey. Remember, knowledge is power, and with the right tools and guidance, managing Cushing syndrome is possible.
Learn more about Cushing Syndrome
See also: 5 Early Signs of Diabetes in Kids
